Leukaemia
An Introduction to Leukaemia
Treating leukaemia holds numerous challenges, including the need for less toxic and more cost-effective treatments. Important additions to the landscape include targeted treatments such as FLT3 inhibitors, BCL-2 inhibitors and immune therapies such as monoclonal antibodies, antibody-drug conjugates and chimeric antigen receptor (CAR) T-cell therapies have been important additions to improve patient outcomes.
Expert video highlights, insights from the conference hub and comprehensive peer-reviewed articles from our journal portfolio provide updates on the changing treatment landscape. To learn more about how the latest developments impact on patient outcomes view our expert-led learning activities.

The European Hematology Association (EHA) has released its official EHA Perspectives in Hematology reports from the 2025 Annual Congress in Milan, now available in two separate editions covering malignant and non-malignant hematology. Following strong interest in the 2024 pilot report, this expanded format offers deeper insights into scientific and clinical advances across the field.
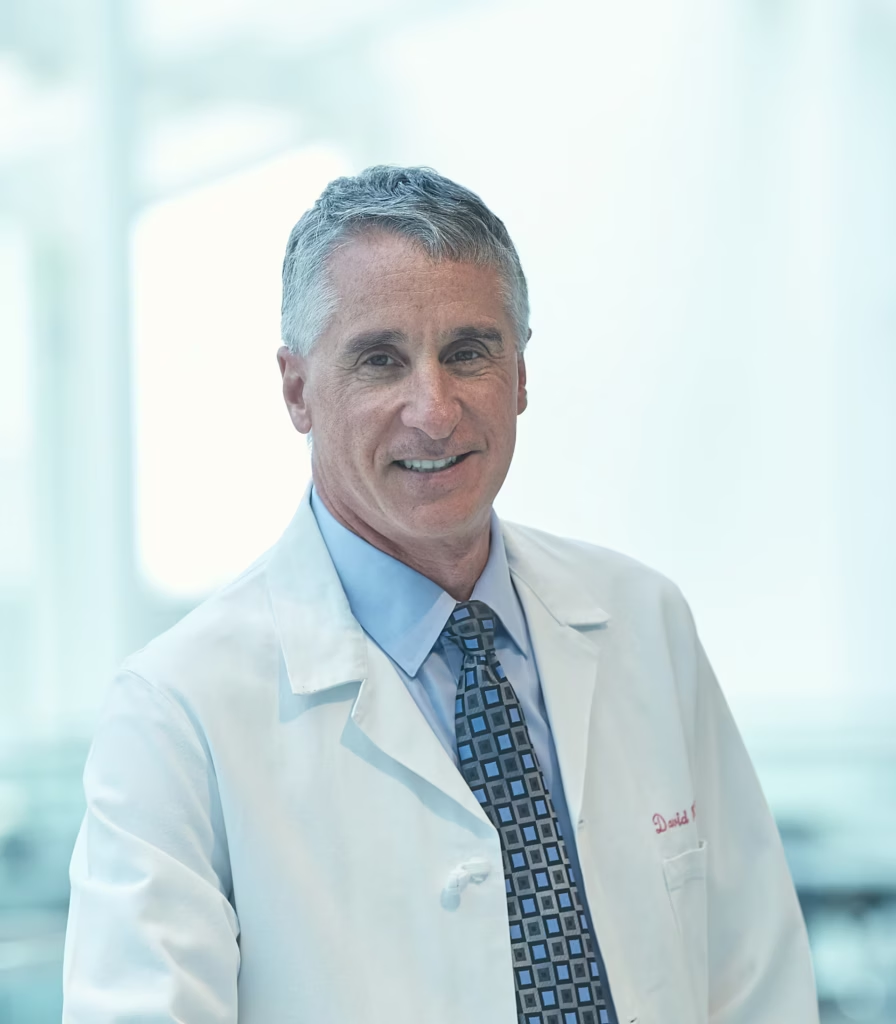
#EHA2025: HARMONY and PETHEMA trials refine AML classification At the 2025 European Hematology Association (EHA) Congress in Milan, new genomic insights challenged current assumptions about acute myeloid leukemia (AML) risk classification. Dr Pinkal Desai (Associate Professor at Weill Cornell Medical College, New York, NY, USA), shares key updates on how next-generation sequencing (NGS) and large-scale data analysis are reshaping the prognostic landscape. In this interview, Dr Desai discusses how the HARMONY Alliance and the PETHEMA registry suggest that a more nuanced genomic framework may better capture individual patient risk. These findings could impact frontline therapy choices, including the potential role of FLT3 inhibitors in core binding factor AML and transplant decisions in NPM1-mutated disease. “I’d like to focus on the evolving classification of acute myeloid leukemia (AML), particularly in light of recent genomic data. Since its publication, the 2022 European LeukemiaNet (ELN) recommendations have guided diagnosis and risk stratification for adult AML patients treated with intensive chemotherapy. However, the landscape is shifting. The growing use of next-generation sequencing (NGS) has enabled broader mutation profiling, leading to new insights into how secondary or co-occurring mutations may influence disease biology and outcomes. HARMONY Alliance study: AI uncovers 17 genomic clusters in AML One abstract that stood out was S148, a HARMONY Alliance study that used AI-based, unsupervised genomic classification in over 4,000 patients with AML treated intensively, with validation from a UK dataset. This analysis revealed 17 molecular clusters within the AML population – each with distinct genomic features and survival implications. A particularly compelling finding involved NPM1-mutated AML, a category now under renewed interest due to the development of menin inhibitors. The study identified three distinct clusters within this subgroup, each associated with different co-mutations and prognoses: NPM1 + FLT3, DNMT3A, or WT1 NPM1 + RAS and PTPN11 NPM1 + IDH2 Each combination carried unique survival outcomes, underscoring the need for greater granularity in risk stratification. Another surprising observation came from patients with core binding factor (CBF) AML, a group typically considered favorable-risk. However, those with FLT3 mutations – primarily FLT3-TKD – had significantly reduced survival compared to CBF patients without FLT3 alterations. Currently, FLT3 inhibitors are not standard in frontline treatment for CBF-AML. This raises important questions: Should FLT3 inhibition be considered in this setting? Could survival improve further with agents like gemtuzumab ozogamicin, which has shown benefit in CBF-AML? The PETHEMA registry refines ELN 2022 with real-world data A second abstract, S146, analyzed data from 1,700 patients in the PETHEMA registry to propose a refined classification based on ELN 2022. The authors suggested dividing patients into four risk groups: favourable, intermediate, adverse and very adverse. One notable insight was that patients with double CEBPA mutations or those harbouring the IDH2 R172H variant had survival similar to traditionally favorable-risk patients – suggesting the latter could be reclassified as favourable, pending validation. The study also re-examined MDS-like secondary mutations, many of which are currently included in the ELN 2022 adverse-risk category. Interestingly, a single MDS-related mutation in the intermediate-risk group did not significantly affect survival. However, two or more such mutations were clearly associated with worse outcomes, both in intermediate and favourable-risk patients. For example, a patient with NPM1-mutated AML – typically favourable – might shift to adverse-risk if they also carry multiple MDS-related mutations, impacting critical decisions like stem cell transplant eligibility. Finally, the proposed very adverse-risk group included patients with TP53 mutations, complex karyotype with TP53 and inversion 3, all associated with extremely poor survival – typically in the range of 6 to 9 months. These studies demonstrate the potential for more precise, genomics-based risk classification in AML, moving beyond the current ELN 2022 framework. The ability to identify distinct genetic subgroups with clear prognostic implications could refine treatment approaches – including the use of targeted therapies and transplant decisions – and ultimately lead to better, more individualized care for patients with AML.” Browse all EHA2025 content here! Disclosure: Pinkal Desai has received grant/research support from Kura Oncology, Janssen Research and BMS. She is a member of the Advisory Board for BMS, Kura Oncology, Syndax, Servier and Abbvie. She has received other financial or material support from Genentech/Roche. Cite: #EHA25: HARMONY and PETHEMA trials refine AML classification. touchHAEMATOLOGY. July xxth, 2025 Interviewer/Editor: Sophie Nickelson This content has been developed independently by Touch Medical Media for touchHAEMATOLOGY. It is not affiliated with the European Hematology Association (EHA). Views expressed are the speaker’s own and do not necessarily reflect the views of Touch Medical Media. SIGN UP to touchHAEMATOLOGY! Join our global community today for access to thousands of peer-reviewed articles, expert insights, and learn-on-the-go education across 150+ specialties, plus concise email updates and newsletters so you never miss out. [bth-register] At EHA 2025, Dr. Pinkal Desai highlighted new genomic insights reshaping AML risk classification. Studies from the Harmony Alliance and PETHEMA registry propose refined groupings based on mutation clusters, challenging existing assumptions – particularly regarding NPM1, FLT3, and MDS-related mutations. These findings may influence both risk assessment and treatment decisions. #EHA2025: HARMONY and PETHEMA trials refine AML classification At the 2025 European Hematology Association (EHA) Congress in Milan, new genomic insights challenged current assumptions about acute myeloid leukemia (AML) risk classification. Dr Pinkal Desai (Associate Professor at Weill Cornell Medical College, New York, NY, USA), shares key updates on how next-generation sequencing (NGS) and large-scale data analysis are reshaping the prognostic landscape. In this interview, Dr Desai discusses how the HARMONY Alliance and the PETHEMA registry suggest that a more nuanced genomic framework may better capture individual patient risk. These findings could impact frontline therapy choices, including the potential role of FLT3 inhibitors in core binding factor AML and transplant decisions in NPM1-mutated disease. “I’d like to focus on the evolving classification of acute myeloid leukemia (AML), particularly in light of recent genomic data. Since its publication, the 2022 European LeukemiaNet (ELN) recommendations have guided diagnosis and risk stratification for adult AML patients treated with intensive chemotherapy. However, the landscape is shifting. The growing use of next-generation sequencing (NGS) has enabled broader mutation profiling, leading to new insights into how secondary or co-occurring mutations may influence disease biology and outcomes. HARMONY Alliance study: AI uncovers 17 genomic clusters in AML One abstract that stood out was S148, a HARMONY Alliance study that used AI-based, unsupervised genomic classification in over 4,000 patients with AML treated intensively, with validation from a UK dataset. This analysis revealed 17 molecular clusters within the AML population – each with distinct genomic features and survival implications. A particularly compelling finding involved NPM1-mutated AML, a category now under renewed interest due to the development of menin inhibitors. The study identified three distinct clusters within this subgroup, each associated with different co-mutations and prognoses: NPM1 + FLT3, DNMT3A, or WT1 NPM1 + RAS and PTPN11 NPM1 + IDH2 Each combination carried unique survival outcomes, underscoring the need for greater granularity in risk stratification. Another surprising observation came from patients with core binding factor (CBF) AML, a group typically considered favorable-risk. However, those with FLT3 mutations – primarily FLT3-TKD – had significantly reduced survival compared to CBF patients without FLT3 alterations. Currently, FLT3 inhibitors are not standard in frontline treatment for CBF-AML. This raises important questions: Should FLT3 inhibition be considered in this setting? Could survival improve further with agents like gemtuzumab ozogamicin, which has shown benefit in CBF-AML? The PETHEMA registry refines ELN 2022 with real-world data A second abstract, S146, analyzed data from 1,700 patients in the PETHEMA registry to propose a refined classification based on ELN 2022. The authors suggested dividing patients into four risk groups: favourable, intermediate, adverse and very adverse. One notable insight was that patients with double CEBPA mutations or those harbouring the IDH2 R172H variant had survival similar to traditionally favorable-risk patients – suggesting the latter could be reclassified as favourable, pending validation. The study also re-examined MDS-like secondary mutations, many of which are currently included in the ELN 2022 adverse-risk category. Interestingly, a single MDS-related mutation in the intermediate-risk group did not significantly affect survival. However, two or more such mutations were clearly associated with worse outcomes, both in intermediate and favourable-risk patients. For example, a patient with NPM1-mutated AML – typically favourable – might shift to adverse-risk if they also carry multiple MDS-related mutations, impacting critical decisions like stem cell transplant eligibility. Finally, the proposed very adverse-risk group included patients with TP53 mutations, complex karyotype with TP53 and inversion 3, all associated with extremely poor survival – typically in the range of 6 to 9 months. These studies demonstrate the potential for more precise, genomics-based risk classification in AML, moving beyond the current ELN 2022 framework. The ability to identify distinct genetic subgroups with clear prognostic implications could refine treatment approaches – including the use of targeted therapies and transplant decisions – and ultimately lead to better, more individualized care for patients with AML.” Browse all EHA2025 content here! Disclosure: Pinkal Desai has received grant/research support from Kura Oncology, Janssen Research and BMS. She is a member of the Advisory Board for BMS, Kura Oncology, Syndax, Servier and Abbvie. She has received other financial or material support from Genentech/Roche. Cite: #EHA25: HARMONY and PETHEMA trials refine AML classification. touchHAEMATOLOGY. July xxth, 2025 Interviewer/Editor: Sophie Nickelson This content has been developed independently by Touch Medical Media for touchHAEMATOLOGY. It is not affiliated with the European Hematology Association (EHA). Views expressed are the speaker’s own and do not necessarily reflect the views of Touch Medical Media. SIGN UP to touchHAEMATOLOGY! Join our global community today for access to thousands of peer-reviewed articles, expert insights, and learn-on-the-go education across 150+ specialties, plus concise email updates and newsletters so you never miss out. [bth-register] At EHA 2025, Dr. Pinkal Desai highlighted new genomic insights reshaping AML risk classification. Studies from the Harmony Alliance and PETHEMA registry propose refined groupings based on mutation clusters, challenging existing assumptions – particularly regarding NPM1, FLT3, and MDS-related mutations. These findings may influence both risk assessment and treatment decisions. At EHA 2025, Dr. Pinkal Desai highlighted new genomic insights reshaping AML risk classification. Studies from the Harmony Alliance and PETHEMA registry propose refined groupings based on mutation clusters, challenging existing assumptions – particularly regarding NPM1, FLT3, and MDS-related mutations. These findings may influence both risk assessment and treatment decisions.
Early-phase AML trials presented at EHA 2025 spotlight promising low-intensity regimens, including menin inhibitor–based triplets and an all-oral decitabine/cedazuridine–venetoclax combination. Dr. Pinkal Desai shares insights on high response rates, manageable safety profiles, and the potential for these regimens to shift the frontline standard of care for vulnerable patients.
At EHA 2025, Dr. Pinkal Desai spotlighted two key developments in younger AML patients: the failure of KIT inhibition in core binding factor AML, and promising early data supporting ziftomenib plus intensive chemotherapy in NPM1-mutated or KMT2A-rearranged AML—signaling a potential shift in frontline treatment strategies.
Daisy Diaz Rohena discusses mechanisms of resistance in high-risk chronic lymphocytic leukemia (CLL), highlighting how relapsed cells maintain BCL2 dependence while upregulating BCL-XL. Her research supports dual targeting as a potential strategy, with WH25244 – a selective BCL-XL degrader – showing preclinical promise. She shares optimism for upcoming translational CLL studies at EHA 2025.

In a study presented at #EHA2025, Dr Ferran Nadeau and colleagues reveal that multiclonality in CLL may be more pervasive – and older – than previously thought. Using single cell sequencing, they identify minor clones carrying CLL-like features and driver mutations decades before diagnosis, suggesting new opportunities for early detection.

Physician burnout is at a critical point. In this episode, Nicky speaks with Dr Alfred Atanda about why so many physicians are burning out and what can be done to change the trend. From personal experience to system-wide solutions, Dr Atanda shares valuable insights on improving physician well-being and building a more effective healthcare culture.
CAR T-cell therapy is transforming blood cancer care, yet most eligible patients never receive it. Dr Miguel-Angel Perales outlines how the CAR T Vision Coalition plans to close this gap.
Learning points:
- Understand why timely referral for CAR T is critical
- Learn how real-world data support broader patient eligibility
- Explore solutions to expand delivery beyond academic centres
- Discover strategies to promote equitable access across regions
Dr. David Porter, President of ASTCT, outlines his vision for the Society’s future, emphasizing expanded access to cell therapies, multidisciplinary collaboration, and a bold strategic plan through 2030. He highlights exciting advances in treating autoimmune diseases and solid tumors, positioning ASTCT to lead in a rapidly evolving therapeutic landscape.
In this episode, we explore the future of continuing medical education (CME) with the team behind touchIME. Hannah Fisher and Matthew Goodwin share insights into global and US trends, the importance of patient inclusivity and how educational outcomes are evolving to better measure the direct impact of learning on clinical practice and patient care.

Dr Zachary Frosch, Fox Chase Cancer Center, shares how patient priorities guide his clinical decisions and how his research stems from real-world challenges. He also reflects on key lessons from mentorship and the ongoing dialogue between the clinic and the research lab that shapes his work.

Dr. Esra Gülderen discusses her path into hematology, the critical role of mentorship, and how early research experiences shaped her confidence. Now a Co-chair of the EBMT Trainee Committee, she shares what motivates her and why clear communication, curiosity, and resilience are essential traits for aspiring haematologists.
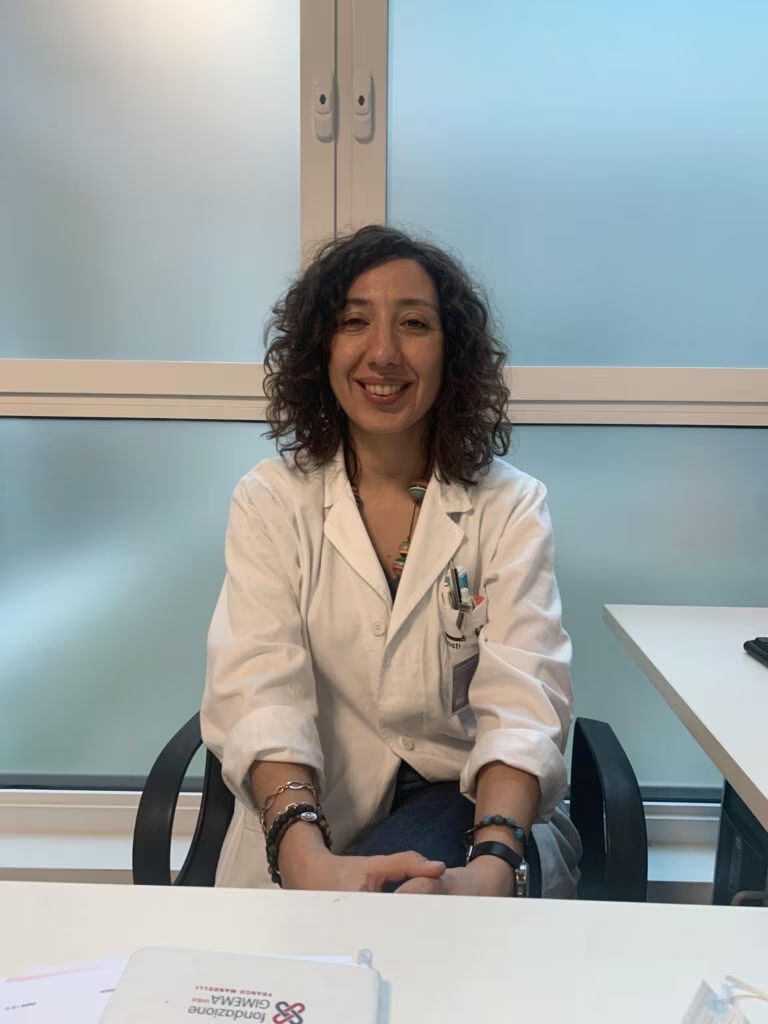
In this interview, Dr Elena Crisà (Candiolo Cancer Institute, FPO-IRCCS, Candiolo, Turin, Italy) shares her insights into the most fulfilling aspects of practicing haematology, from working in cutting-edge new treatment options in clinical trials to guiding patients through complex treatment decisions.
CD7-targeted CAR T-cell therapy, WU-CART-007, demonstrates encouraging anti-leukemic activity and a manageable safety profile in heavily pretreated patients with relapsed/refractory (R/R) T-cell acute lymphoblastic leukemia/lymphoblastic lymphoma (T-ALL/LBL). This updated analysis from the phase II portion ...
Latest articles videos and clinical updates - straight to your inbox
Log into your Touch Account
Earn and track your CME credits on the go, save articles for later, and follow the latest congress coverage.
Register now for FREE Access
Register for free to hear about the latest expert-led education, peer-reviewed articles, conference highlights, and innovative CME activities.
Sign up with an Email
Or use a Social Account.
This Functionality is for
Members Only
Explore the latest in medical education and stay current in your field. Create a free account to track your learning.





