#EHA2025: HARMONY and PETHEMA trials refine AML classification
At the 2025 European Hematology Association (EHA) Congress in Milan, new genomic insights challenged current assumptions about acute myeloid leukemia (AML) risk classification. Dr Pinkal Desai (Associate Professor at Weill Cornell Medical College, New York, NY, USA), shares key updates on how next-generation sequencing (NGS) and large-scale data analysis are reshaping the prognostic landscape. In this interview, Dr Desai discusses how the HARMONY Alliance and the PETHEMA registry suggest that a more nuanced genomic framework may better capture individual patient risk. These findings could impact frontline therapy choices, including the potential role of FLT3 inhibitors in core binding factor AML and transplant decisions in NPM1-mutated disease.
“I’d like to focus on the evolving classification of acute myeloid leukemia (AML), particularly in light of recent genomic data. Since its publication, the 2022 European LeukemiaNet (ELN) recommendations have guided diagnosis and risk stratification for adult AML patients treated with intensive chemotherapy. However, the landscape is shifting. The growing use of next-generation sequencing (NGS) has enabled broader mutation profiling, leading to new insights into how secondary or co-occurring mutations may influence disease biology and outcomes.
HARMONY Alliance study: AI uncovers 17 genomic clusters in AML
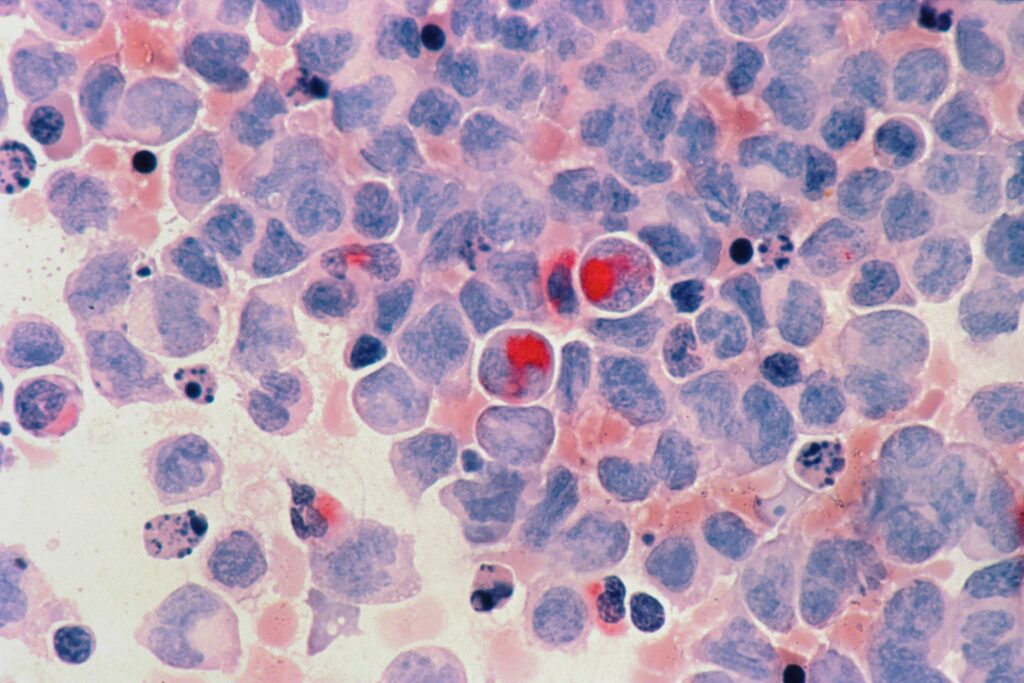
One abstract that stood out was S148, a HARMONY Alliance study that used AI-based, unsupervised genomic classification in over 4,000 patients with AML treated intensively, with validation from a UK dataset. This analysis revealed 17 molecular clusters within the AML population – each with distinct genomic features and survival implications.
A particularly compelling finding involved NPM1-mutated AML, a category now under renewed interest due to the development of menin inhibitors. The study identified three distinct clusters within this subgroup, each associated with different co-mutations and prognoses:
NPM1 + FLT3, DNMT3A, or WT1
NPM1 + RAS and PTPN11
NPM1 + IDH2
Each combination carried unique survival outcomes, underscoring the need for greater granularity in risk stratification. Another surprising observation came from patients with core binding factor (CBF) AML, a group typically considered favorable-risk. However, those with FLT3 mutations – primarily FLT3-TKD – had significantly reduced survival compared to CBF patients without FLT3 alterations. Currently, FLT3 inhibitors are not standard in frontline treatment for CBF-AML. This raises important questions:
Should FLT3 inhibition be considered in this setting?
Could survival improve further with agents like gemtuzumab ozogamicin, which has shown benefit in CBF-AML?
The PETHEMA registry refines ELN 2022 with real-world data
A second abstract, S146, analyzed data from 1,700 patients in the PETHEMA registry to propose a refined classification based on ELN 2022. The authors suggested dividing patients into four risk groups: favourable, intermediate, adverse and very adverse.
One notable insight was that patients with double CEBPA mutations or those harbouring the IDH2 R172H variant had survival similar to traditionally favorable-risk patients – suggesting the latter could be reclassified as favourable, pending validation.
The study also re-examined MDS-like secondary mutations, many of which are currently included in the ELN 2022 adverse-risk category. Interestingly, a single MDS-related mutation in the intermediate-risk group did not significantly affect survival. However, two or more such mutations were clearly associated with worse outcomes, both in intermediate and favourable-risk patients. For example, a patient with NPM1-mutated AML – typically favourable – might shift to adverse-risk if they also carry multiple MDS-related mutations, impacting critical decisions like stem cell transplant eligibility.
Finally, the proposed very adverse-risk group included patients with TP53 mutations, complex karyotype with TP53 and inversion 3, all associated with extremely poor survival – typically in the range of 6 to 9 months.
These studies demonstrate the potential for more precise, genomics-based risk classification in AML, moving beyond the current ELN 2022 framework. The ability to identify distinct genetic subgroups with clear prognostic implications could refine treatment approaches – including the use of targeted therapies and transplant decisions – and ultimately lead to better, more individualized care for patients with AML.”
Browse all EHA2025 content here!
Disclosure: Pinkal Desai has received grant/research support from Kura Oncology, Janssen Research and BMS. She is a member of the Advisory Board for BMS, Kura Oncology, Syndax, Servier and Abbvie. She has received other financial or material support from Genentech/Roche.
Cite: #EHA25: HARMONY and PETHEMA trials refine AML classification. touchHAEMATOLOGY. July xxth, 2025
Interviewer/Editor: Sophie Nickelson
This content has been developed independently by Touch Medical Media for touchHAEMATOLOGY. It is not affiliated with the European Hematology Association (EHA). Views expressed are the speaker’s own and do not necessarily reflect the views of Touch Medical Media.
SIGN UP to touchHAEMATOLOGY!
Join our global community today for access to thousands of peer-reviewed articles, expert insights, and learn-on-the-go education across 150+ specialties, plus concise email updates and newsletters so you never miss out.
[bth-register]
At EHA 2025, Dr. Pinkal Desai highlighted new genomic insights reshaping AML risk classification. Studies from the Harmony Alliance and PETHEMA registry propose refined groupings based on mutation clusters, challenging existing assumptions – particularly regarding NPM1, FLT3, and MDS-related mutations. These findings may influence both risk assessment and treatment decisions.
#EHA2025: HARMONY and PETHEMA trials refine AML classification
At the 2025 European Hematology Association (EHA) Congress in Milan, new genomic insights challenged current assumptions about acute myeloid leukemia (AML) risk classification. Dr Pinkal Desai (Associate Professor at Weill Cornell Medical College, New York, NY, USA), shares key updates on how next-generation sequencing (NGS) and large-scale data analysis are reshaping the prognostic landscape. In this interview, Dr Desai discusses how the HARMONY Alliance and the PETHEMA registry suggest that a more nuanced genomic framework may better capture individual patient risk. These findings could impact frontline therapy choices, including the potential role of FLT3 inhibitors in core binding factor AML and transplant decisions in NPM1-mutated disease.
“I’d like to focus on the evolving classification of acute myeloid leukemia (AML), particularly in light of recent genomic data. Since its publication, the 2022 European LeukemiaNet (ELN) recommendations have guided diagnosis and risk stratification for adult AML patients treated with intensive chemotherapy. However, the landscape is shifting. The growing use of next-generation sequencing (NGS) has enabled broader mutation profiling, leading to new insights into how secondary or co-occurring mutations may influence disease biology and outcomes.
HARMONY Alliance study: AI uncovers 17 genomic clusters in AML
One abstract that stood out was S148, a HARMONY Alliance study that used AI-based, unsupervised genomic classification in over 4,000 patients with AML treated intensively, with validation from a UK dataset. This analysis revealed 17 molecular clusters within the AML population – each with distinct genomic features and survival implications.
A particularly compelling finding involved NPM1-mutated AML, a category now under renewed interest due to the development of menin inhibitors. The study identified three distinct clusters within this subgroup, each associated with different co-mutations and prognoses:
NPM1 + FLT3, DNMT3A, or WT1
NPM1 + RAS and PTPN11
NPM1 + IDH2
Each combination carried unique survival outcomes, underscoring the need for greater granularity in risk stratification. Another surprising observation came from patients with core binding factor (CBF) AML, a group typically considered favorable-risk. However, those with FLT3 mutations – primarily FLT3-TKD – had significantly reduced survival compared to CBF patients without FLT3 alterations. Currently, FLT3 inhibitors are not standard in frontline treatment for CBF-AML. This raises important questions:
Should FLT3 inhibition be considered in this setting?
Could survival improve further with agents like gemtuzumab ozogamicin, which has shown benefit in CBF-AML?
The PETHEMA registry refines ELN 2022 with real-world data
A second abstract, S146, analyzed data from 1,700 patients in the PETHEMA registry to propose a refined classification based on ELN 2022. The authors suggested dividing patients into four risk groups: favourable, intermediate, adverse and very adverse.
One notable insight was that patients with double CEBPA mutations or those harbouring the IDH2 R172H variant had survival similar to traditionally favorable-risk patients – suggesting the latter could be reclassified as favourable, pending validation.
The study also re-examined MDS-like secondary mutations, many of which are currently included in the ELN 2022 adverse-risk category. Interestingly, a single MDS-related mutation in the intermediate-risk group did not significantly affect survival. However, two or more such mutations were clearly associated with worse outcomes, both in intermediate and favourable-risk patients. For example, a patient with NPM1-mutated AML – typically favourable – might shift to adverse-risk if they also carry multiple MDS-related mutations, impacting critical decisions like stem cell transplant eligibility.
Finally, the proposed very adverse-risk group included patients with TP53 mutations, complex karyotype with TP53 and inversion 3, all associated with extremely poor survival – typically in the range of 6 to 9 months.
These studies demonstrate the potential for more precise, genomics-based risk classification in AML, moving beyond the current ELN 2022 framework. The ability to identify distinct genetic subgroups with clear prognostic implications could refine treatment approaches – including the use of targeted therapies and transplant decisions – and ultimately lead to better, more individualized care for patients with AML.”
Browse all EHA2025 content here!
Disclosure: Pinkal Desai has received grant/research support from Kura Oncology, Janssen Research and BMS. She is a member of the Advisory Board for BMS, Kura Oncology, Syndax, Servier and Abbvie. She has received other financial or material support from Genentech/Roche.
Cite: #EHA25: HARMONY and PETHEMA trials refine AML classification. touchHAEMATOLOGY. July xxth, 2025
Interviewer/Editor: Sophie Nickelson
This content has been developed independently by Touch Medical Media for touchHAEMATOLOGY. It is not affiliated with the European Hematology Association (EHA). Views expressed are the speaker’s own and do not necessarily reflect the views of Touch Medical Media.
SIGN UP to touchHAEMATOLOGY!
Join our global community today for access to thousands of peer-reviewed articles, expert insights, and learn-on-the-go education across 150+ specialties, plus concise email updates and newsletters so you never miss out.
[bth-register]
At EHA 2025, Dr. Pinkal Desai highlighted new genomic insights reshaping AML risk classification. Studies from the Harmony Alliance and PETHEMA registry propose refined groupings based on mutation clusters, challenging existing assumptions – particularly regarding NPM1, FLT3, and MDS-related mutations. These findings may influence both risk assessment and treatment decisions.
At EHA 2025, Dr. Pinkal Desai highlighted new genomic insights reshaping AML risk classification. Studies from the Harmony Alliance and PETHEMA registry propose refined groupings based on mutation clusters, challenging existing assumptions – particularly regarding NPM1, FLT3, and MDS-related mutations. These findings may influence both risk assessment and treatment decisions.







 touchHAEMATOLOGY
touchHAEMATOLOGY