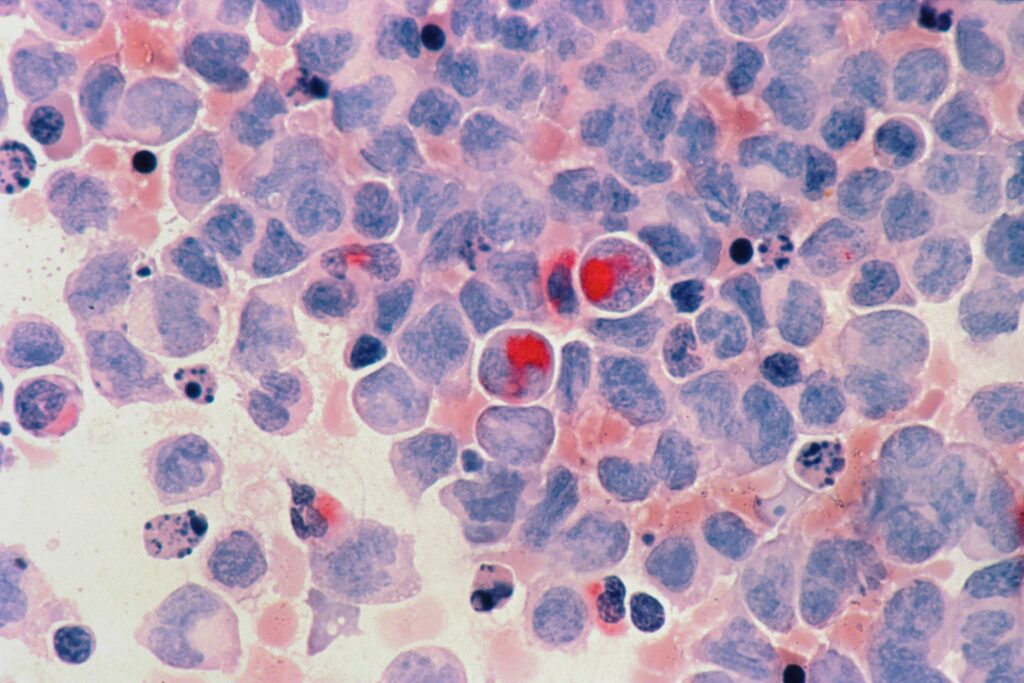
“We are facing an exciting era of fast-paced drug development in acute myeloid leukaemia” writes Gianfranco Bittar and colleagues at Baylor College of Medicine, Houston, TX, USA, in a review published in touchREVIEWS in Oncology & Haematology. In 2020, there were an estimated 21,450 new patients with acute myeloid leukaemia (AML) and 11,180 AML-related deaths in the USA. Rates of complete remission (CR) with the standard ‘7+3’ regimen (that is, continuous intravenous infusion of cytarabine for 7 days plus an anthracycline for the first 3 days) range from 55% to 60% in patients younger than 70 years, and from 40% to 45% in older patients.
In recent years, researchers have worked towards “genetically characterizing AML to provide a more accurate prognosis, personalize management and develop targeted therapies”, the authors write; they note that the United States Food and Drug Administration (FDA) has now approved several agents against specific molecular targets, which have improved outcomes. The authors summarize the promising clinical trials that may advance AML management.
Midostaurin, a multikinase inhibitor originally developed for the treatment of solid tumours, was approved by the FDA in 2017 in combination with standard induction chemotherapy for FLT3-positive AML. This followed results of the RATIFY phase III trial, in which patients with concurrent NPM1 mutations had a 5-year overall survival rate of approximately 70% in the midostaurin group. Use of high-dose cytarabine plus midostaurin, followed by autologous haemopoietic stem cell transplant (aHSCT) also shows potential, following the results of the phase II German–Austrian AML Study Group 16-10 trial, in which 72.4% of patients achieved CR/CR with incomplete haematological recovery (CRi).
For elderly patients with comorbidities, intensive treatment can lead to complications such as differentiation syndrome. The authors suggest that IDH1 inhibitors as add-on maintenance therapy alongside hypomethylating agents (HMAs) in patients with CR after intense chemotherapy, or HMA plus venetoclax induction, could be a treatment option for these patients, citing ongoing trials.
Patients older than 75 years and those with significant comorbidities are best treated with HMA plus venetoclax, the authors suggest, citing a recent study by DiNardo et al., in which the combination demonstrated a CR/CRi rate of 66% in the overall population. Venetoclax 600 mg plus low-dose cytarabine 20 mg/m2 daily for 10 days was approved by the FDA in 2020. Following the positive results of the phase III QUAZAR AML-001 trial, the FDA approved oral azacitidine (CC-486) as a maintenance therapy.
In summary, although clinical outcomes for patients with AML have improved over the past 5 years, there are still urgent therapeutic needs to consider. These include:
- The need to improve induction therapy for patients with de novo AML in adverse European LeukemiaNet (ELN) 2017 subgroups, and for those with relapsed/refractory (R/R) AML.
- Drug designs that permit oral HMA with improved pharmacodynamics, to improve leukaemia-free survival in patients without a donor or those who are unsuitable for aHSCT.
- Novel drug combinations that can prevent primary and secondary failure of HMA plus BCL2 inhibitor combination therapy, are needed.
- Interventions that improve the relapse risk after bone marrow transplantation, especially in patients in intermediate-risk/adverse ELN subgroups, must be identified.
The authors offer an overview of promising future therapeutic options, including:
- magrolimab in combination with azacitidine (which showed promising results in a phase Ib trial among patients with TP53-mutated AML)
- combination of azacitidine, venetoclax and magrolimab in patients with R/R AML (following positive phase I/II data)
- HMA plus venetoclax, which has been shown to be particularly effective in inducing negative measurable residual disease
- maintenance therapy (oral azacitidine), following the favourable results of the QUAZAR AML-001 trial.
“We are facing an exciting era of fast-paced drug development in AML”
“As leukaemia-treating physicians, we should continue to encourage clinical trial participation and foster the integration of basic and clinical science to improve the lives of patients with AML” the author conclude.
Read the full article by Gianfranco Bittar and colleagues on touchONCOLOGY:
Advances and Future Goals in Acute Myeloid Leukaemia Therapy
touchREVIEWS in Oncology & Haematology. 2022;18(2):130-8 DOI: https://doi.org/10.17925/OHR.2022.18.2.130