“Some patients don’t have one CLL – they have nine”
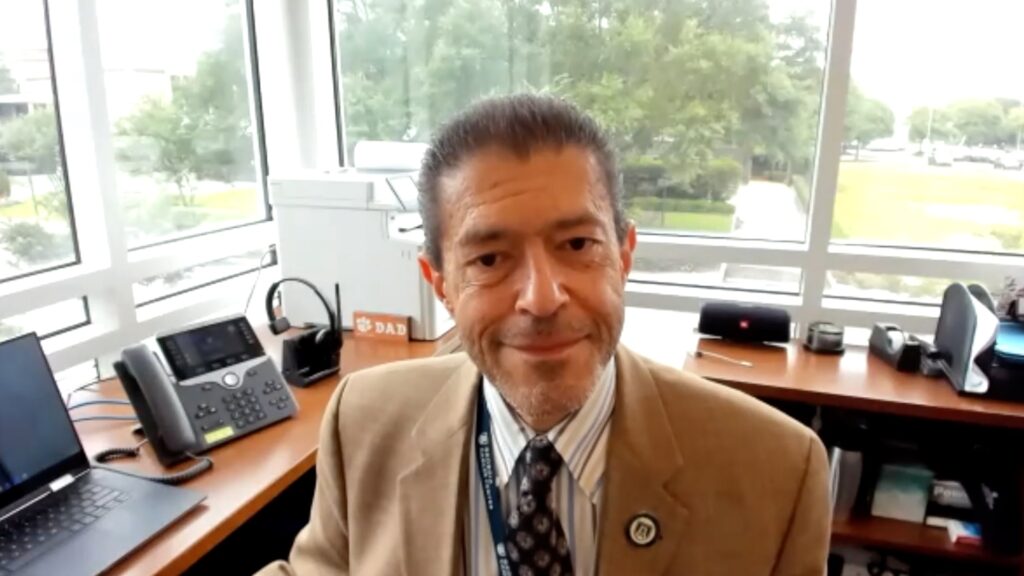
A new study presented at #EHA2025 by Dr Ferran Nadeu (Post-doctoral researcher, Hospital Clínic de Barcelona, Barcelona, Spain) et al. offers a comprehensive look at multiclonality in chronic lymphocytic leukemia (CLL). By applying advanced single cell sequencing across a large cohort of patients, the team reveals that minor clones with CLL-like features can emerge decades before diagnosis – raising questions about early detection and disease predisposition.
The plenary abstract, ‘MINOR INDEPENDENT CLONES IN PATIENTS WITH CHRONIC LYMPHOCYTIC LEUKEMIA HAVE A CLL-BIASED BIOLOGICAL SIGNATURE: IMPLICATIONS FOR DISEASE ONTOGENY AND EVOLUTION’ (Abstract: S204) was presented at the European Hematology Association (EHA) 2025 Congress from June 12-15th in Milan, Italy.
Q1. What led you to explore multiclonality in CLL?
We started studying multiclonality in CLL because it offers a unique and fascinating opportunity to observe how different B cell neoplasms – not different diseases, but clones from the same disease entity – grow within the same individual. It’s a rare setting where we can explore whole tumours evolving in parallel.
By focusing specifically on CLL, studying multiclonality brings us closer to understanding the disease’s origin. It’s been known for some years that multiclonality is present in around 10% of CLL cases, but it’s even more common in early disease stages, such as monoclonal B cell lymphocytosis (MBL), both low-count and high-count forms.
So our aim was to better understand the extent of multiclonality, which is still poorly characterized, and to gain insight into the early events that drive the disease. This includes early genetic and transcriptomic changes that may occur during these initial phases.
Q2. Please describe the main aims of your study
Polyclonality is observed in about 20–30% of early-stage cases and around 10% of CLL cases. We wanted to study this more comprehensively in a larger patient cohort, to define the extent of multiclonality and characterize minor clones – even those that are not significantly expanded. Beyond simply describing the clonal architecture – the number and size of different B cell clones – we aimed to analyze their molecular features using new single cell technologies. These allow us to study their transcriptomic profiles as a proxy for phenotype, as well as any genomic alterations.
We also wanted to explore the evolutionary relationships among these clones: whether they arise from a common ancestor or from entirely different cells of origin.
Q3. What was the methodology and eligibility criteria?
We included samples from patients diagnosed with CLL, as well as from those with low- or high-count MBL, provided suitable samples were available for analysis. So the inclusion criteria were relatively broad. To contextualize our findings, we also studied over 120 age-matched healthy individuals. This allowed us to compare B cell architecture in CLL patients with that in healthy people.
We started with deep sequencing of the immunoglobulin gene, which serves as a marker for clonal B cells. All B cells derived from a single clone share the same immunoglobulin gene rearrangement. We performed this sequencing in more than 300 CLL patients and in 120 healthy individuals.
In selected cases with interesting multiclonality patterns, we conducted further analyses using single cell RNA sequencing to profile the transcriptome, single cell DNA sequencing to detect driver alterations, and a new protocol for single cell whole genome sequencing. This last approach allowed us to construct phylogenetic trees – like those used to study species evolution – to trace the development of different clones over time, offering a retrospective view of their emergence throughout the patient’s life.
Q4. Please can you summarize the results and key takeaways?
In line with previous studies, we found that around 12% of CLL cases exhibit oligoclonality – that is, multiple distinct CLL clones with different immunoglobulin gene rearrangements. This has been described before, but our study provides new insight.
What’s novel is that even minor clones – those not significantly expanded – show a biased pattern of immunoglobulin gene rearrangement when compared with healthy individuals. These minor clones in CLL patients already exhibit immunogenetic features similar to CLL, suggesting that the entire B cell repertoire is skewed toward a CLL-like phenotype.
Using single cell RNA sequencing, we confirmed that many of these small clones also have a CLL transcriptomic profile. Genetically, many carried driver mutations typically seen in CLL – some associated with aggressive disease, such as TP53 mutations or IGLV3-21 R110 mutations – despite their small size.
Interestingly, in some patients, the dominant clone lacked detectable driver mutations, while minor clones carried high-risk alterations. That was unexpected.
With single cell whole genome sequencing, we analyzed more than 150 individual cells from different patients and reconstructed the evolutionary history of their clones. We found that many of these clones do not share any somatic mutations, indicating independent origins from distinct cells.
This approach also allowed us to estimate when the driver mutations occurred. In some cases, these alterations were acquired decades before diagnosis – sometimes before the age of 30 – even in patients diagnosed at 60 or 70. These clones started to grow 10–20 years before the disease becomes clinically apparent.
To give one example, we identified up to nine distinct CLL clones in a single patient – not just one CLL, but nine co-existing CLL clones. Some of these were very small, but they already exhibited the transcriptomic and genetic hallmarks of CLL.
Q5. What might this mean for the future of CLL early detection and clinical practice?
In terms of clinical practice, we’re still some way from applying these findings directly. But by studying how and why multiple CLL clones emerge in some individuals – and not in others – we may uncover key insights into the disease’s origins.
There’s evidence suggesting a genetic or epigenetic predisposition to developing CLL, and our research could help identify early alterations or drivers. By understanding when these changes occur and how the disease develops over time, we move closer to building a more dynamic picture of CLL – not just at diagnosis, but over the course of decades.
This could open up new possibilities for early detection in individuals who are predisposed, and perhaps, eventually, for early intervention strategies.
Q6. What key presentations are you most excited for at EHA 2025?
It’s hard to choose – there have been so many interesting and well-executed studies. Within the CLL field, there are some excellent sessions on disease biology and new or updated therapies that are changing the treatment landscape.
Beyond CLL, there are exciting advances in immunotherapy and lymphomas. And from a scientific and technological perspective, the sessions on single cell technologies are particularly compelling. As this study shows, these tools are helping us to better understand tumour evolution and immune dynamics, and will hopefully lead to improved diagnostics and treatment in the future.
Browse all EHA2025 content here!
Disclosure: Dr Ferran Nadeu has no financial or non-financial conflicts of interest in relation to this article.
Cite: #EHA2025: Multiclonality in CLL: New Insights into Early Evolution and Detection. touchHAEMATOLOGY. June 25th, 2025
Interviewer: Caroline Markham
This content has been developed independently by Touch Medical Media for touchHAEMATOLOGY. It is not affiliated with the European Hematology Association (EHA). Views expressed are the speaker’s own and do not necessarily reflect the views of Touch Medical Media.
SIGN UP to touchHAEMATOLOGY!
Join our global community today for access to thousands of peer-reviewed articles, expert insights, and learn-on-the-go education across 150+ specialties, plus concise email updates and newsletters so you never miss out.