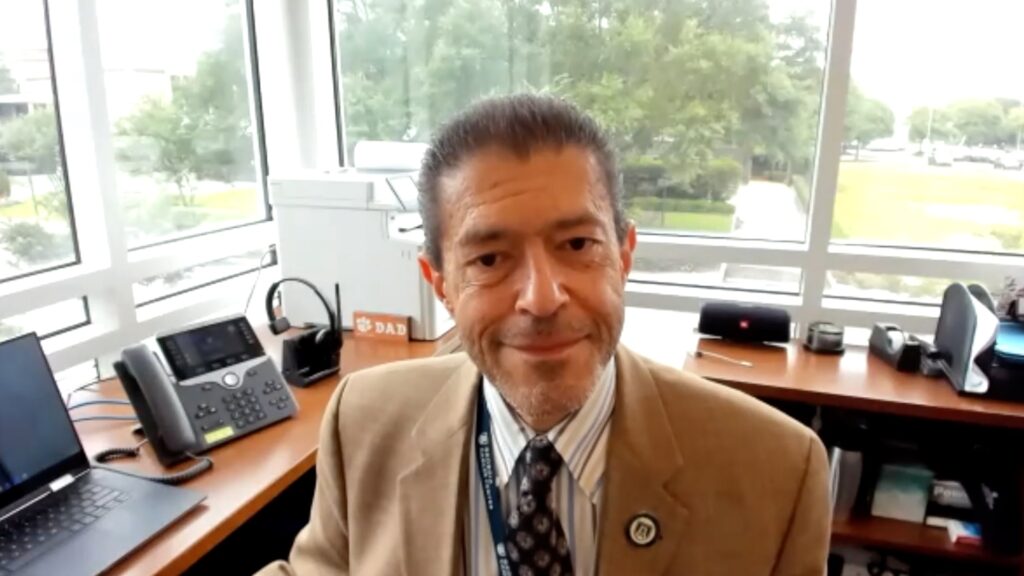
In this interview, Prof. Robin Foà, a distinguished haematologist and now Emeritus Professor of Haematology at the Sapienza University of Rome, Italy, shares the inspirations and career-defining moments that led him to focus on haematology and leukaemia research. Initially trained in paediatrics, Prof. Foà’s interest in blood disorders began with early work on haemoglobinopathies, eventually leading him to specialize in haematology. His time at London’s Hammersmith Hospital in the late 1970s profoundly shaped his career. There, he worked with renowned figures such as his mentor Prof. Daniel Catovsky.
Prof. Foà reflects on his legacy, emphasizing the importance of supporting the next generation of haematologists and enhancing translational research. He discusses major advancements in treating haematological malignancies, including the transformative role of tyrosine kinase inhibitors and immunotherapy. He highlights the challenges in making these therapies accessible globally. In closing, he offers advice for aspiring haematologists, underscoring both the rewards and challenges of a career in this evolving field.
Q1. What motivated or inspired you to specialise in haematology, and more specifically leukaemia?
Well, it’s interesting. I first specialized in paediatrics in the 1970s, and then moved into haematology. I graduated at the University of Turin, north-west of Italy. During my first year of medicine, I qualified as a ski instructor and during the winter I taught skiing during the weekends and holidays in Bardonecchia. I then specialised in paediatrics. During this time, I started working on hemoglobinopathies, mainly thalassemia and sickle cell disease, then on children with leukaemia, and this developed my interest in haematology.
I began working in the laboratory, particularly on the in vitro growth of myeloid colonies, and started to realize the importance and potential of research. I decided to move abroad, and chose London because I have family in England and London was pioneering at the time in research into haematological malignancies. I spent 3 years between 1976 and 19799 at the MRC Leukaemia Unit, Royal Postgraduate Medical School, Hammersmith Hospital, which was a unique environment, and proved to be a turning point for me in haematology and my subsequent professional career.
Why did I move into leukaemia research? Largely, because I was working in a unit called the MRC Leukaemia Unit and because of the influence of the top individuals below. At the time, Hammersmith Hospital was one of the centres of the world in haematology research, and I was very fortunate to work with some of the most renowned and pioneering haematologists.
My mentor was Prof. Daniel Catovsky, a globally recognized researcher and physician, who made significant advancements in the diagnosis and classification of haematological cancers, particularly in the fields of hairy cell leukaemia and chronic lymphocytic leukaemia (CLL). His wife, Dame Julia Margaret Polak, was a research histopathologist and one of the longest-surviving recipients of a heart-lung transplant in the UK. They both became very dear and valued friends.
Danny Catovsky had an interest in chronic lymphoproliferative disorders (CLDs), the most frequent of which is CLL, which is the most common leukaemia in the Western world. He was one of the main players in CLDs and CLL, recognized worldwide. So, I started working in this area and found it very interesting. And so, my clinical interest shifted from paediatrics to adults, as CLL is a disease that exists only in adults and mainly in elderly.
Another prominent senior figure was Sir John Dacie, first Professor of Haematology in the UK in 1956, at Royal Postgraduate Medical School, Hammersmith Hospital, and a leader in haemolytic anaemias. He is best known for discovering and naming Christmas disease, now commonly called haemophilia B. Sir John was the founder of the Leukaemia Research Unit at Hammersmith Hospital in 1969 and served as the founding editor of the British Journal of Haematology.
Prof. David Abraham Goitein Galton, a pioneer in developing effective treatments for adult patients with leukaemia and lymphoma, was Professor of Haemato-Oncology and Chair of the Medical Research Council. Prof. John Goldman was also at Hammersmith Hospital. He conducted some of the first bone marrow transplants in Europe and was a world-known expert in chronic myeloid leukaemia (CML), a disease for which he conducted pioneering research into the development of the drug imatinib.
Q2. Do you have any advice for young, aspiring haematologists, and what do you want your legacy to be?
I am lucky to have had a very full and varied career, and I think it’s our duty to foster the younger generations as much as possible. Haematology is a beautiful discipline because it combines laboratory research and clinical practice. It is important that the younger generations not only appreciate the beauty of the discipline but recognize that it’s a tough path to go down. There is a lot of studying in university and hospital, alongside clinical and laboratory work. It is not necessarily a discipline or specialty that allows a route into an active private practice or to make large incomes, but if you have the dreams and the goals, it can be an extremely rewarding career. Over the years, my work has allowed me (and still allows me) to work in Italy (Turin and Rome), UK (London) and the USA (New York), and to interact with colleagues all over the world, many becoming close friends.
I have been a member of the European Hematology Association (EHA) since the beginning in 1992. I was President of the society in 2009 to 2011 and Chairman of the Education Committee from 2013 to 2017 and set up the Outreach Unit in 2017. We implemented education programs for younger generations of haematologists around the world, not only in Central Europe, in conjunction between EHA and national societies of the different countries. All the programs were tailored according to the local realities and what could be of value and useful for them.
From London, I returned to Turin where my academic career developed. Between 1991 and 1992, I spent a year in New York at Memorial Sloan Kettering Cancer Center. I then moved to Rome to be Professor of Haematology and head of the Haematology Centre at the Sapienza University of Rome. There, with the fundamental help of my wife Anna (Rita) Guarini, we set up many laboratories necessary for the clinic and I continued my research in the enhancement of translational research in leukaemia. This has been a key focus on my career ever since, and another fundamental legacy for the future of haematological malignancies.
A final thought for the younger generations. For me, haematology has been a privilege that holds even today. Work can offer side opportunities; for example, it allowed me over the years to foster my hobby of photography. An invitation for a lecture tour in China that materialized back in 1985 and took us (my wife and I had just married) to visit many parts of China. Many years later, this became China 1985, my second photography book.1,2
Q3. Reflecting on your career, what have been the most exciting advances in the treatment of haematological malignancies?
When I look back at the last 40 years of treatment for haematological malignancies, the advances have been fascinating. Overall survival rates were much lower. As an example, 20 years ago – before the use of tyrosine kinase inhibitors (TKIs) – patients with CML had a median life expectancy of around 3.5–4 years. Nowadays, median life expectancy is approaching that of people of the same age without leukaemia. Another example comes from acute promyelocytic leukaemia, which nowadays can be mostly controlled without chemotherapy. All of this stems from research and advancement in knowledge.
Over the years, much of my research has been in acute lymphoblastic leukaemia (ALL), particularly Philadelphia chromosome-positive (Ph+) ALL. This is an illuminating story; from being the worst haematologic tumour (and possibly cancer), to today curing most patients of all ages, many without chemotherapy or transplant, using targeted treatment with a TKI plus immunotherapy with the monoclonal antibody blinatumomab. In the last 25 years, I have worked on clinical trials researching the use of TKIs in Ph+ ALL and we were the first to use a TKI for all patients without chemotherapy. Years ago, this would have been unbelievable.
So, things have changed dramatically, and we are today treating and curing patients with haematological malignancies with less chemotherapy and transplant through a progressively growing personalized and targeted management pathway. The future will only get better and brighter thanks to an ever closer link between the clinic and the laboratories.
Q4. What can you see being the main challenges in making these new treatment strategies available around the world?
This is a very important point. There is so much out there talking about the most advanced medicine, but real life is very different from the more fortunate patients living in lucky, first-world countries, particularly if recruited in clinical trials. Non-chemotherapy drugs are not available in most parts of the world, so they are still using the old treatment: chemotherapy, with all the toxicities and adverse effects. Many of the drugs are phenomenally expensive, which isn’t sustainable in global populations; gene therapy, for example, is around €3 million per patient. How many patients can access CAR-T cells? So, while the future is bright, the real-life issues, like costs and accessibility to drugs and technologies, are very concerning. We’re moving forward quickly, but we would like that optimal management – that in many cases is life-saving – is made available to as many patients as possible.
More information
- Foà R. China 1985: Photographs by Robin Foà. Fidenza: Mattioli 1885, 2012.
- Robin Foà Photographer. Home. Available at: https://robinfoa.it/ (accessed date: 15 November 2024).
Disclosures: Robin Foà has no financial or non-financial conflicts of interest to declare in relation to this article.
Cite: Foà R. A legacy in haematology: Prof. Robin Foà’s path from paediatrics to global impact. touchHAEMATOLOGY. 19 November, 2024.