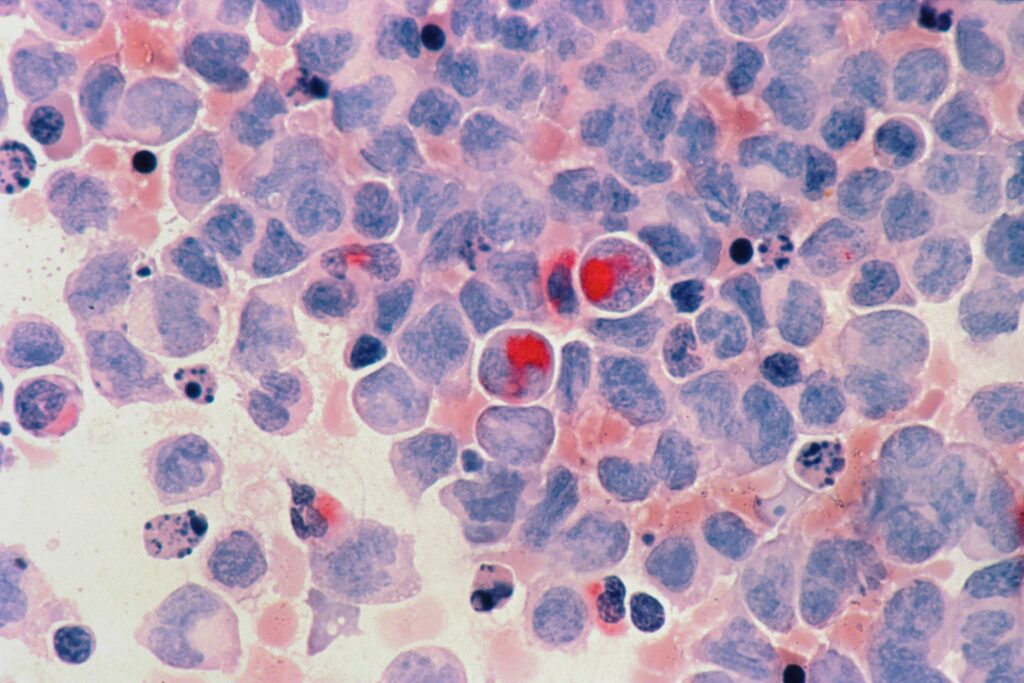
Histone-lysine N-methyltransferase 2A rearrangements (KMT2Ar) and mutant nucleophosmin 1 (mNPM1) occur in approximately 5–10% and 30% of patients with acute myeloid leukaemia (AML), respectively.1,2 Both mutations are associated with the founding events in the development of leukaemia.1 In particular, KMT2Ar functions in a protein complex requiring menin, leading to the deregulation of genes, including homeobox A cluster (HoXA), and cooperates with NPM1, leading to the dysregulation of leukaemogenic genes.1
Currently, there are no approved targeted therapies for AML with KMT2Ar or mNPM1, and disease outcomes remain poor with standard therapies.3,4 However, research is underway to develop treatments targeting KMT2A and NPM1, and key clinical data of novel treatments for patients with relapsed/refractory (R/R) AML were presented at the 2022 American Society of Hematology Annual Meeting in New Orleans, LA, USA, in December 2022. Prof. Jorge Cortes from the Georgia Cancer Center at Augusta University (August, GA, USA) provided an overview of two studies that may lead to advances in the treatment of these types of AML.
The first study Prof. Cortes discussed was the phase I AUGMENT-101 trial (ClinicalTrials.gov identifier: The median patient age was 43 (range: 1–79), and patients had received a median of 4 (range: 1–12) prior lines of therapy, with 46% of patients having had a prior transplant. Grade 3 QTc prolongation was found to be dose-limiting toxicity (DLT) with treatment, and grade 2 differentiation syndrome was reported in 16% of patients; grade ≥3 treatment-related adverse events were not frequent (2–3%) and included diarrhoea, fatigue, anaemia, tumour lysis syndrome, neutropenia, thrombocytopenia, hypercalcemia and hypokalaemia.
After a median follow-up of 4.6 months (range: 0.3–21.9), the overall response rate (ORR) in the overall efficacy population of 60 patients was 53%, with patients with KMT2Ar and mNPM1 having an ORR of 59% and 36%, respectively; the complete response (CR)/CR with partial haematologic recovery (CRh) rates in these groups were 30%, 33% and 21%, respectively. The median duration of response was 9.1 months (95% confidence interval [CI]: 2.7–not reached), and the median overall survival was 7.0 months (95% CI: 4.3–11.6). As these results are promising, enrolment in the phase II AUGMENT-101 study is now on-going.
The second study Prof. Cortes discussed was the phase I/II KOMET-001 trial (ClinicalTrials.gov identifier: NCT04067336) assessing the impact of another inhibitor of the KMT2A–menin interaction, ziftomenib.6 In the dose-escalation phase Ia part of the study, 30 adults with R/R AML of any genotype, 33% and 13% of whom had , received 50–1000 mg ziftomenib.
In the dose-validating phase Ib part of the trial, the 200 and 600 mg doses from phase Ia were assessed in 24 patients with KMT2A. In this phase, the median patient age was 46 years (range: 31–82); the median number of prior therapies was 2.5 (range: 1.0–12.0) in the 200 mg group and 4.0 (range: In total, seven patients developed differentiation syndrome, four of which were grade ≥3 events, including one death. Grade ≥3 treatment-related adverse events occurring in more than 10% of patients included anaemia (25%), febrile neutropenia (25%), neutropenia (25%), thrombocytopenia (25%), differentiation syndrome (17%), leukocytosis (17%), sepsis (13%) and leukopenia (13%). Preliminary efficacy data suggested that ziftomenib treatment effects were dose dependent. With the 200 mg dose, stable or decreasing blast counts and changes in bone marrow morphology were observed, and both the ORR and the CR/CRh were 0.0%. In patients receiving the 600 mg dose, the ORR was 41.7% (95% CI: 15.2–72.3), and the CR/CRh rate was 25.0% (95% CI: 5.5–57.2). As of the data cut-off, 50% of patients remained on treatment.
In conclusion, the results for revumenib and ziftomenib suggest that both inhibitors may be promising treatment options for patients with R/R AML, an area of great unmet need. Further research is required to determine the efficacy and safety of these treatments as monotherapies and in combination.
The full meeting interview with Prof. Jorge Cortes is available on touchONCOLOGY here.
The 2022 American Society of Hematology Annual Meeting abstracts mentioned in this article are available at the following links: